Welcome to the 2025 Winter edition of our CU MFM e-newsletter! Here we focus on the trending topic of mental health in pregnancy and postpartum. We are excited to introduce our new perinatal mental health preconception clinic as well as a pivotal new postpartum depression study in which our division is participating.
CU Maternal-Fetal Medicine Winter 2025 Newsletter
Perinatal Mental Health Preconception Clinic
The CU Maternal-Fetal Medicine division has launched a new Perinatal Mental Health Preconception Clinic that will be led by Katherine (Kate) McMeekin, WHNP-BC, MSN. This clinic is dedicated to serving individuals who are considering, actively planning for pregnancy or newly pregnant and have a history of mental health conditions. These conditions include anxiety, depression, OCD, PTSD, ADHD, bipolar disorder, schizophrenia and more. Our goal is to provide comprehensive, personalized care to help patients navigate this exciting and complex journey, ensuring their mental health is prioritized every step of the way. These consultations will be offered virtually to allow for patients all around Colorado to easily access this service.
Through this clinic, we guide patients in understanding the risks and benefits of their current medications and therapies as well as make recommendations that may be most appropriate for them. We work to develop a tailored plan that optimizes their mental health before conception. By working together, we can create a foundation for a healthy pregnancy, both mentally and physically. This program is intended to be collaborative amongst Maternal-Fetal Medicine (MFM) specialists, OB providers, and mental health professionals to provide seamless, multidisciplinary care. This will ensure that patients are supported throughout their pregnancy and beyond, with their treatment plans thoughtfully maintained.
We know that individuals with psychiatric conditions are at a higher risk of experiencing unintended pregnancies, which can often exacerbate mental health challenges. Recognizing this, the clinic will also provide early pregnancy consultations to create proactive management plans customized to each patient's unique circumstances. Our goal is to prevent exacerbations of mental health conditions and promote the well-being of both the patient and their baby.
This clinic represents a unique opportunity to address a critical gap in care and empower patients with the knowledge, resources, and synergistic care they need to embrace pregnancy while prioritizing their mental health confidently. We believe this program will significantly help women's health providers and their patients as they navigate this transformative time during pregnancy.
To refer a patient or for more information, call 303-315-6100 or fax 303-468-3481.
Learn more about Kate:

Senior Instructor
Postpartum Depression Study
Dr. Camille Hoffman, MFM, is partnering with Reunion Neuroscience on a study evaluating whether a single dose of a psilocybin analogue can improve symptoms of Postpartum Depression (PPD). PPD is a major form of depression that is estimated to affect roughly 10-15% of all mothers of newborns. Women suffering from PPD often experience significant changes in mood, appetite and sleep contributing to feelings of hopelessness, lack of concentration, loss of energy, poor self-esteem and maternal disinterest.
There is only one current therapy approved specifically for PPD, Zuranolone. This medication is taken as a 14-day course, at bedtime, due to side effects that include sedation. SSRIs, which are often prescribed off-label, take a long time for onset and only show limited efficacy.
While there have been recent developments in treatment options for PPD, there continues to be an unmet need for a solution that offers a faster onset of action, greater efficacy after only a single dose, with limited interruption in breast feeding and a faster return to normal daily activities.
To learn more about the study or to refer a patient to the study team, email Camille.Hoffman-Shuler@CUAnschutz.edu or Jocelyn.Phipers@CUAnschutz.edu.
Recommendation for Vasa Previas
Vasa previas, best diagnosed by endovaginal ultrasound, carry significant fetal morbidity/mortality risk. This risk is dramatically reduced when diagnosed prenatally, as compared to postnatally.
Most vasa previas (60%) at term occur in the context of a resolved previa or low-lying placenta. As such, endovaginal ultrasound with color Doppler is recommended for ALL patients presenting for follow-up of placental location (prior placenta previa or low-lying placenta) even if abdominal ultrasound suggests that the placenta is >2cm from the cervix.
Figure 3. Transvaginal ultrasound scan with color Doppler image and pulsed wave Doppler image shows fetal heart rate
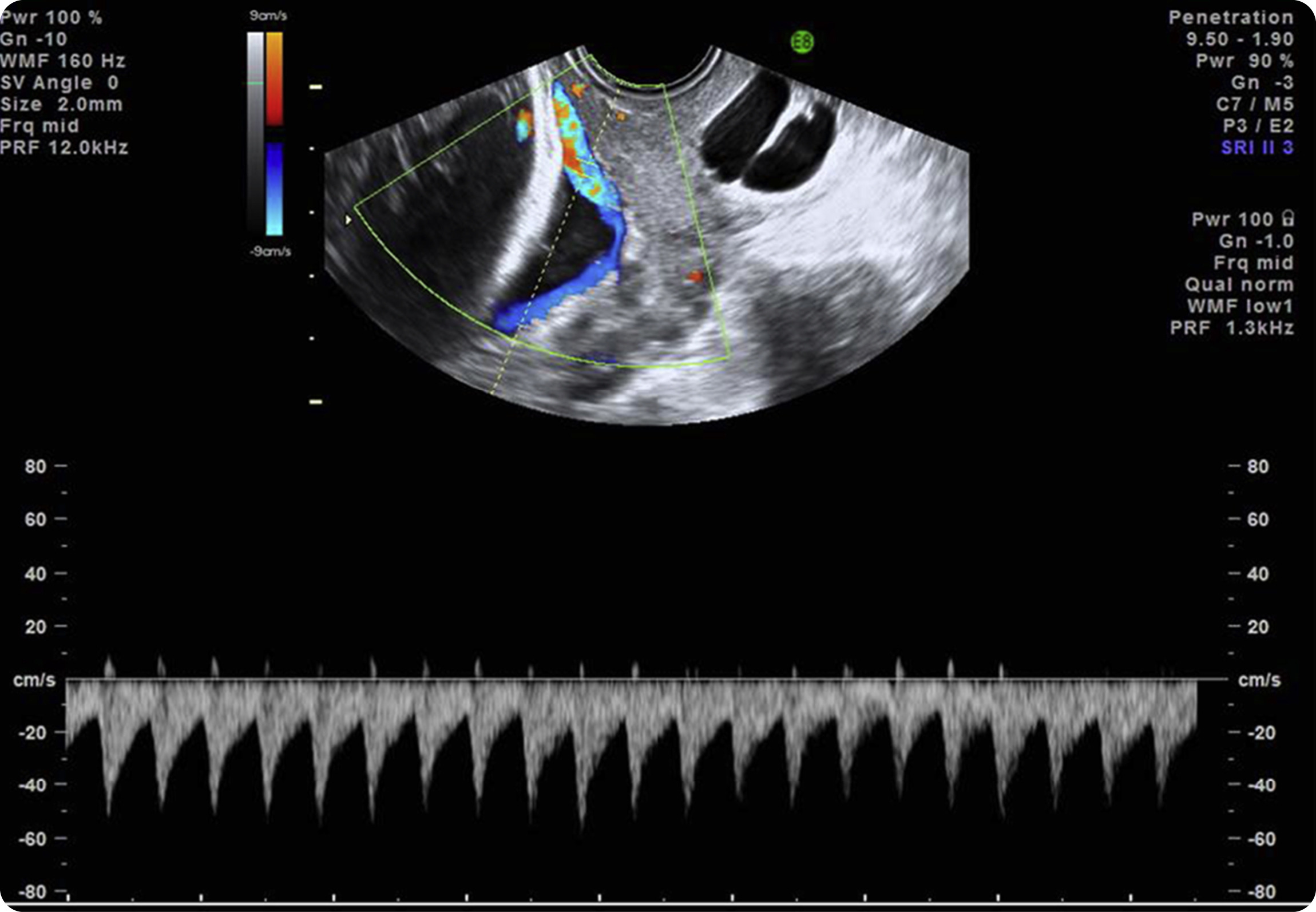 Pulsed wave Doppler of the vessel over the cervical os depicts a fetal heart rate, confirming a diagnosis of vasa previa.
Pulsed wave Doppler of the vessel over the cervical os depicts a fetal heart rate, confirming a diagnosis of vasa previa.
Source: SMFM. Diagnosis and management of vasa previa. Am J Obstet Gynecol 2015.
News You Can Use
DocLine wait times have increased for all service lines to the University of Colorado. Measures are being taken to address the issue. We will continue to provide the utmost care and attention when our referring community utilizes this number.
Addressing Perinatal Mental Health
Join us for our next virtual CME series presented by Kate McMeekin, WHNP-BC, MSN on Wednesday, January 22nd as she discusses “Addressing Perinatal Mental Health”. Visit the link below for information and to register for CME credit.
Join us at SMFM 2025
Denver is the host city for the annual Society for Maternal-Fetal Medicine Pregnancy Meeting occurring January 27th to February 1st at Gaylord Rockies Resort and Convention Center. Many specialists from our program will present abstracts and posters. For more information and to register for this conference, visit the link below.
We Value Your Feedback!
We invite you to share your thoughts, experiences and suggestions related to our content and services. Do you have any questions or topics you'd like us to cover in future editions or educational events? Are there any success stories or challenges in Maternal-Fetal Medicine that you'd like to see featured? Have you experienced issues, concerns or discrepancies with our services? Please email Kelly Clark, Kelly.Clark@ChildrensColorado.org, or fill out our online form. Your input helps us tailor our content and educational offerings to better serve your needs and interests. Join the conversation and be a part of shaping our community!